Using risk adjustment for better patient outcomes
Healthcare organizations need to balance the high costs of treating America’s high volume of chronic conditions
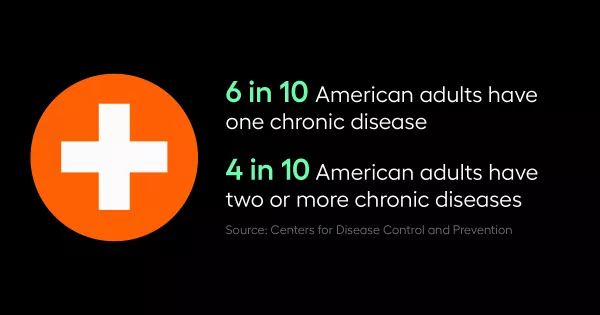
From depression to obesity to diabetes, 60% of U.S. adults have a chronic condition, with 40% having two or more. Care of sick patients is costly. It hurts providers, payers, and patients. To manage these chronic conditions and balance out the high costs of treating them, healthcare organizations are turning to risk adjustment. Risk adjustment is a statistical method that seeks to predict a person’s likely use and cost of healthcare services. Based on a person’s health status, they are assigned a risk score designed to predict healthcare costs.
“Providers want to take care of the sick patients, but they're also required to meet quality and cost initiatives. And they don't want to look like they're not getting their patients better and it's costing a lot. So, risk adjustment helps balance that out for them. On the payer side it helps give them a little incentive to actually cover these people. For patients, it is hard to get coverage when you're sick, or have a heavy disease burden. So, risk adjustment helps balance that out and provides a win-win-win for patient, payer, and provider.” explains Mann.
In 2021, BILHPN launched a pilot program to provide more focused training and education to providers to accurately reflect the health statuses of its patients and attribute them appropriately.
“We like to focus on both the application side and the provider side,” explained Smith. “From an application side, we target those trainings towards either providers when they're at the point of care, but we also focus on application training for staff, whether that's a provider organization, or a specific risk unit, to make sure that they're aware of how to help the care team to drive some of these complexities in the workflow that need to also get done.”
Anna Basevich, Vice President of Enterprise Partnerships at Arcadia, Victoria Smith, Director of Process Improvement and Design at Beth Israel Lahey Health Performance Network, and Maria Mann, Clinical Product Manager at Arcadia discuss how risk adjustment drives population outcomes, and specifically, what Beth Israel Lahey Health Performance Network (BILHPN) has done in the Arcadia webinar, Risk Adjustment Tactics.
Risk adjustment and comprehensive documentation
Risk adjustment programs rely on comprehensive documentation. Chronic conditions need to be assessed at provider visits and those assessments need to be documented. However, this can be challenging for providers who have short windows of time to spend with each patient.
“Because documentation in any kind of way is not taught in medical school, it is up to us to gear providers into why they're doing this,” explained Mann. “And the complete picture is always important. It's not just about risk adjustment; it's about complete capture of conditions. And if it's all there, then the quality of care is improved.”
In addition, Basevich adds that it's important to express that idea of a complete picture to providers during training.
“It's also about having that comprehensive medical record and ensuring that if the primary care physician can't be in the day that the patients being seen, if the patient shows up in the ER, they show up at the specialist, everyone seeing that patient has the right understanding of their context and can provide the most appropriate care,” she said.
Designing a program takes a village
One of the challenges of risk adjustment is that there are a lot of moving parts. Doing it well takes a village – you need proper engagement from physicians, care teams, coding teams, compliance, and more. Begin to design a program by answering who, what, when, where, why, and how. What risk models do you want to cover and why are usually easy first questions to answer. The who (what stakeholders need to be involved), when, and how (what tools you will use) get more complicated to answer.
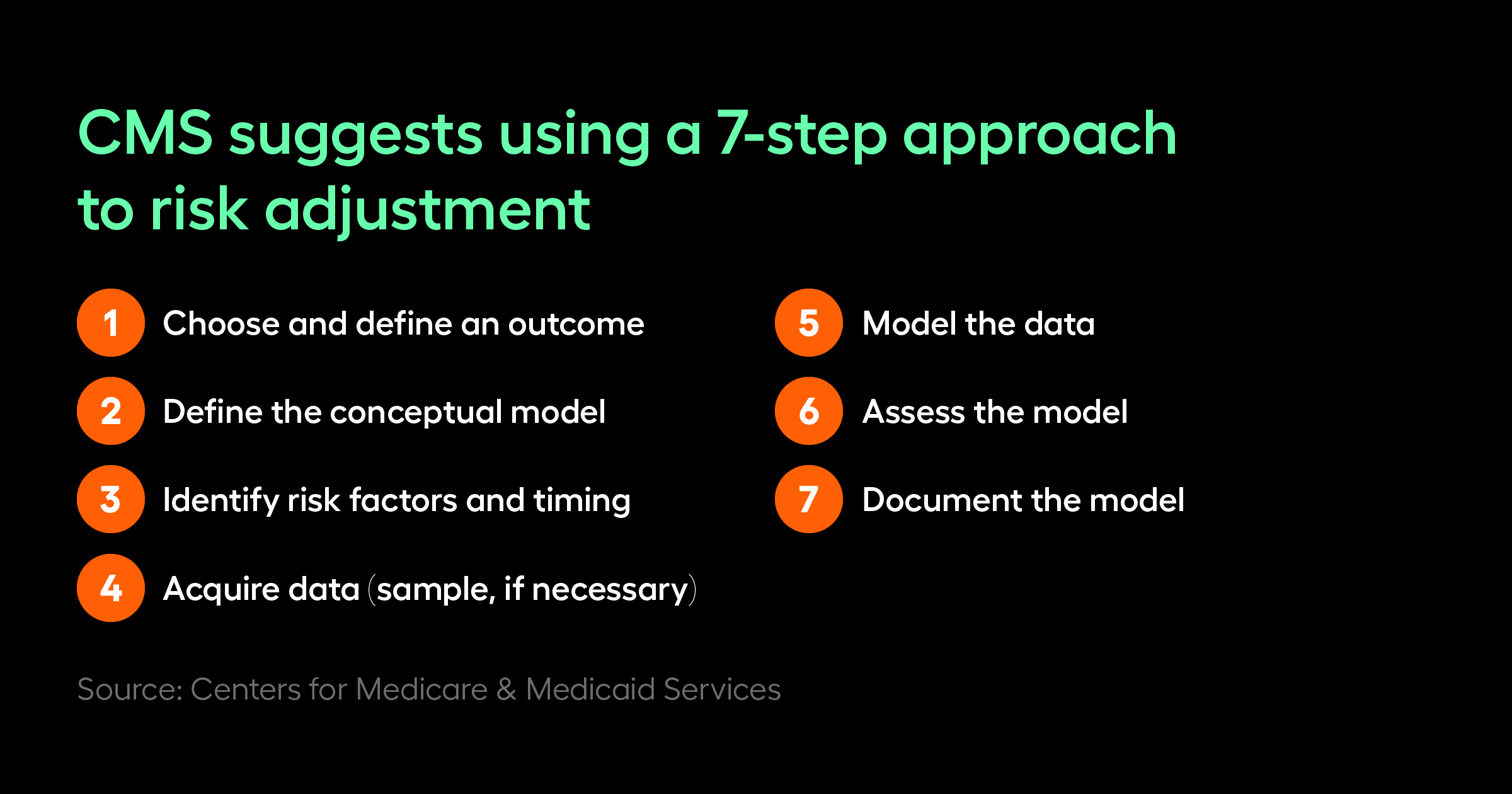
The Centers for Medicare and Medicaid Services recommends a 7-step process for designing a risk adjustment program.
- Choose and define an outcome
- Define the conceptual model
- Identify risk factors and timing
- Acquire data
- Model the data
- Assess the model
- Document the model
Mann recommends selecting tools that make the process as efficient as possible and deliver key performance metrics at both the high-level and granular level.
Next, develop a pilot program as a proof of concept in order to gather lessons learned and expand accordingly.
“One of the largest things we have drawn on for this is the planning stages and breaking it down into digestible pieces. We were able to look through the data and target specific sites that we needed to focus on and hone in on each to see what that impact would be,” said Smith. “When we launched these at the micro level, we learned a lot more about potential barriers or issues up that frontline and within those respective workflows that we could address than otherwise looking at it from a macro view we may not have been able to uncover.”
Finally, select a provider champion at each practice that can act as a translator for your program for the other providers and really support its goals.
Parallels and integrations with other organizational teams
Risk adjustment programs bring complexity, and that can sound daunting and risky for organizations just getting started, but you can draw on organizational strengths and learn lessons from other programs.
BILHPN links to its quality team, reporting team, and billing/coding teams.
“We link with our quality team in order to collaborate whenever needed,” said Smith. “Another area is reporting – we have a quality and risk registry; we also have quality gap reports and try to integrate that data where we're able to. And then of course billing – all of the diagnoses get sent out on a claim and all services also get sent out on the claim, so working with billing teams and coding teams in that same aspect to see where we can align and integrate.”
Engaging resources boils down to why this matters
Expect pushback from providers in particular, because let’s be honest, there’s not a lot of people who think that documenting the same condition over and over is their highest calling. One role of the training programs is to help win the hearts and minds of physicians.
“At the end of the day, a lot of what we're doing is driving change management on why this matters. And we know from decades of training organizations on all kinds of similar topics, that that's half the battle, and that in a lot of cases, you’ve got to hear that message from a lot of different points of view,” said Smith.
At BILHPN, the pilot model has been helpful because it created peers that have done it as the program expands. “The pilot model creates providers and practice staff who can say, ‘this wasn't something that I was necessarily psyched about from day one. Here's how I approached it; here are the challenges I faced; and here's what I liked about the outcome,’” she noted.
Mann adds that you can set up a healthy competition between providers on who's better or more engaged, that can drive more engagement from your lower performing providers because nobody wants to be at the bottom of the list.
BILHPN blends their approach to remain agile in its feedback.
“We send the performance depending upon the program, but for most of our programs we send performance where providers are able to see others and in other cases, we send overall metrics in regards to perhaps our risk unit. So, it might not be at the provider level, but at a risk level or at a practice level,” said Smith.
By looking at engagement rates, BILHPN can also determine why it isn't being used in the way it needs to.
“We might go to a specific provider meeting and get additional feedback, understand the barriers and from that, we might understand that we need one-on-one sessions, but we also need that feedback loop to see if the way that we're showing performance or reviewing performance is actually getting through the transparency or importance of the initiative, as well as driving the results we want to see,” concluded Smith.
Measuring success is never cookie cutter
Measurement for risk adjustment is never going to be one-size-fits-all. It varies from organization to organization and within organizations as well. The most important piece of measurement is identifying what you want to get from the metrics.
“Really focus on what you are trying to get from the metrics, not just to put numbers up to put numbers up, but what is that actionable stuff you take from that? And at what level do you actually need to intervene?” said Smith.
She says what works best is looking at key KPIs and understanding if you need to dig deeper and then implementing appropriate strategies for the specific situations.
“If it's an across-the-board issue, or if it's a practice issue or provider issue; how you'd follow up on those would be different,” said Smith. “You might be able to say, I know that we have the most open gaps in the depression, severe obesity and diabetes area with all the different diabetes diagnoses and this looks like it's across the board. So, you may want to implement a strategy around that that's more at that macro level.”
In addition, internal coding audits for education purposes are essential and will alert you to the need for more documentation or coding education.
“You have to have a system set up where you are reviewing the coding so that you can see before it actually becomes an issue on an external audit,” said Mann.
Finally, use anecdotal feedback to track specific conditions that need to be addressed, or what might be the toughest areas that providers need more awareness around.
“We identify it based upon any anecdotal feedback and through our dashboards in regards to what conditions we may need to focus on, so we do a two-pronged approach of having both qualitative and quantitative analysis to be able to drive those agendas,” explained Smith.
Use BILHPN as a model for inspiration
BILHPN is a model for strong risk adjustment programs. Understanding their thoughtful approach can help other healthcare organizations develop programs that really drive better patient outcomes.
Learn more about risk adjustment offerings and explore ways to close risk gaps.



