Using data to lower A1Cs and drive advances in diabetes treatment
With 60% of the American adult population currently battling a chronic disease such as diabetes, managing them has become a significant part of what healthcare organizations do on a daily basis. WakeMed Key Community Care, an accountable care organization in Raleigh, North Carolina that serves about 200,000 members, has engaged in two pilot programs designed to control diabetes in their population with continuous glucose monitoring (CGM).
In Arcadia’s Byte-Sized Insights, Jon O’Neil, Director of Analytics and IS at WakeMed spoke with Nicole DeCoudres, PA-C, Director of Client Business Management at Arcadia to explain how these programs aim to show that CMG can lower patients’ A1Cs.
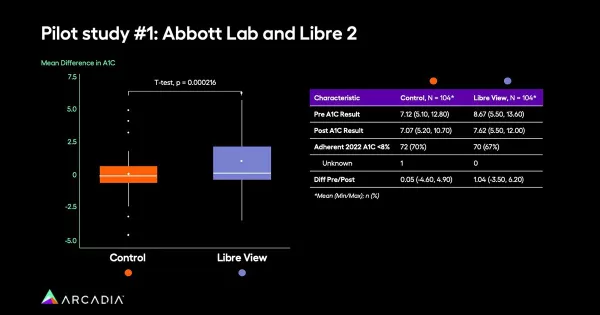
Pilot Program 1: Abbott Lab and Libre 2
Libre 2 is a continuous glucose monitoring system. Abbott Lab gave free access to the system for six weeks to a sample of 300 Type 1 or Type 2 diabetes patients at WakeMed.
WakeMed used historical data from Arcadia about the patients’ past A1C draws both pre and post having the Libre 2 CGM installed. It found 104 people who had received the device had A1C draws within three months receiving it and also within six months of stopping use of the device, so O’Neil and his team developed a quasi-experiment that looked at A1C numbers and how people with the CGM compared to a control group.
“Fortunately, we had the foundation database where we could show some really interesting results by creating a control group after the fact,” said O’Neil.
The results of the analysis showed that the people who received the Libre 2 saw a reduction of 1% in their A1C, while the control group saw a .05% reduction in A1C.
“It appears from this information that people who were given this device did a lot more to reduce their A1C over the period of the study,” said O’Neil.
DeCoudres added that knowledge is power.
“When you know what your glucose level is all the time, you’re less likely to eat that sugary meal or more likely to exercise,” she said.
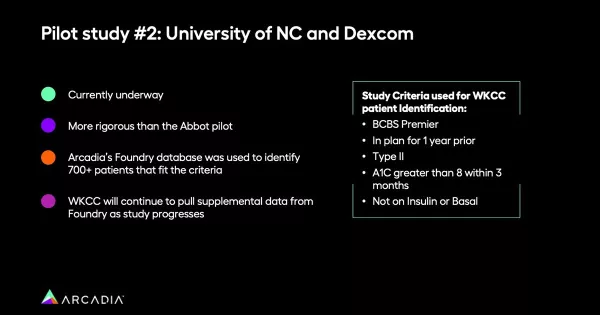
Pilot 2: University of North Carolina and Dexcom
The second program is currently underway. It is a larger, more rigorous study run by the University of North Carolina to explore using Dexcom continuous glucose monitoring for Type 2 diabetes patients who have never been on insulin. The goal was to see if Type 2 diabetics benefit from this system—if they actively monitor their blood sugar will they decrease their A1C?
“Right now, insurance will only cover CGMs for Type 1’s on insulin, but you can make the case through data that you [patients with Type 2 diabetes] can lower your A1C,” said DeCoudres.
WakeMed pulled a random sample from its population for the study and provided patient information to UNC’s public health department and Dexcom for their analysis. O’Neil found providers within their network who are eager to use the systems and identified 700 patients that could qualify for the study. They are now in the phase of recruiting those patients to the study. The hope is that the results of the study will be published in a medical journal upon its completion.
Using data to drive advances in treatment
Providers need better ways to manage their patients’ chronic conditions. By using data to investigate future treatments, diabetes and many other diseases can be well-controlled and patients can live longer, happier lives. Request a demo to see how we can put your data to work, together.
